Why are GP Practices merging?
07-12-2018

"There is arguably no more important job in modern Britain than that of the family doctor. GP's are by far the largest branch of British medicine. A growing and ageing population, with complex multiple health conditions, means that personal and population-orientated primary care is central to any country's health system. As a recent British Medical Journal headline put it 'if general practice fails, the whole NHS fails'.â€
Unfortunately the NHS and in particular General Practice is under increasing pressure. There is currently a divergence in that there is an aging / elderly population with increasingly complex health needs requiring more time and continuity in a system with decreasing resources, social care and community support. General Practice is being asked to provide better access with improved opening times whilst having a recruitment and retention crisis.
Surgeries are collapsing and the unthinkable is happening, surgeries are closing as they are no longer sustainable.
There are therefore 2 options:
1. Continue the status quo. Comfort is taken from a system that is understood. However, in doing this we must acknowledge that there is a significant risk that Primary Care will not continue in its current guise.
2. Innovate and look at system wide change. This is difficult but provides a service that looks after the patient as a whole and is not fragmented and disjointed by the need to use different providers in the community.
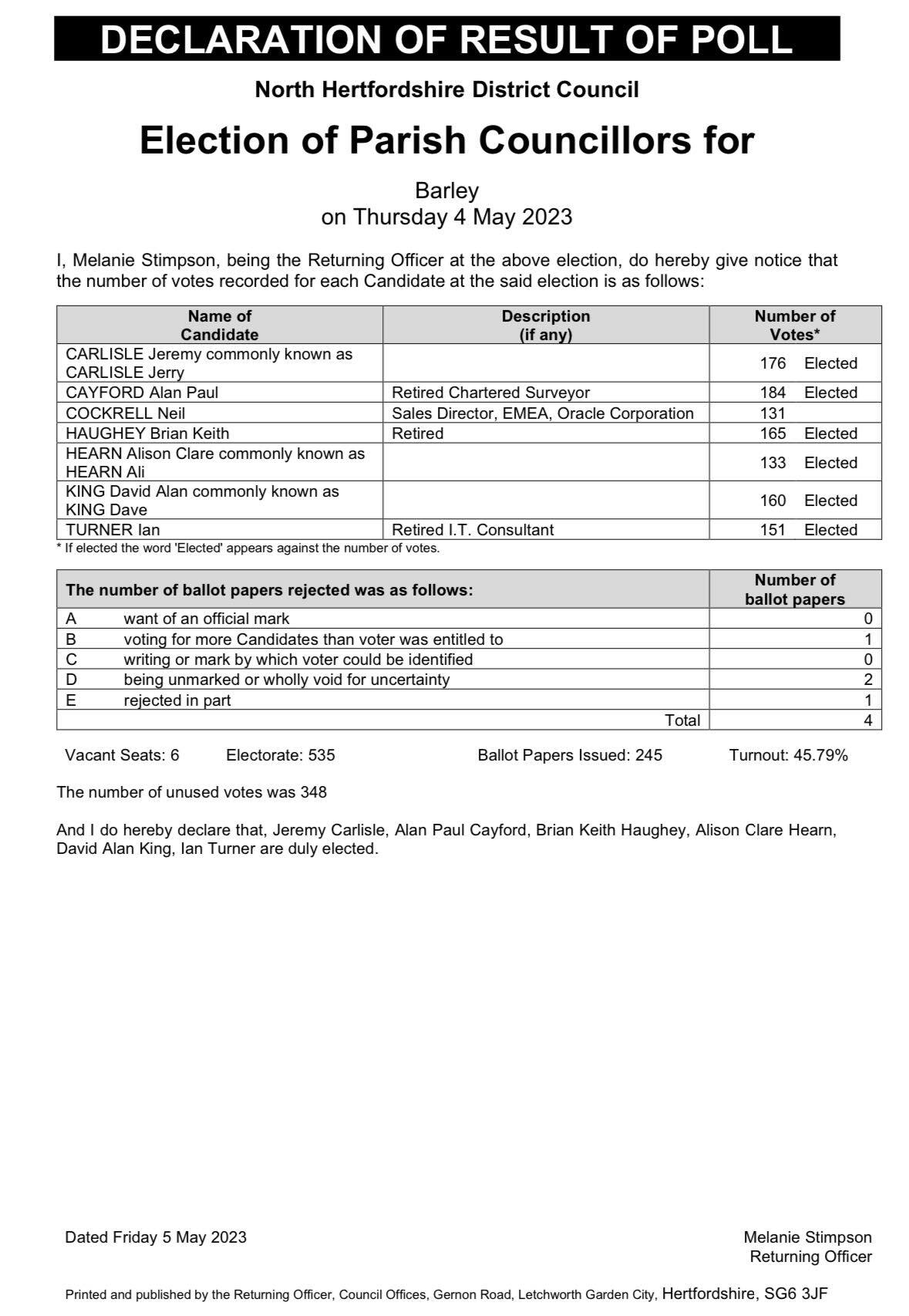
With the mergers of Sawston, Linton, Barley and Shelford, Granta Medical Practices are addressing this struggle with a view to becoming a Primary Care Home. This provides stability as a practice, increased internal skills, and an increased ability to adapt to change. This then becomes more attractive to the multi-disciplinary teams as a place to work, removing the recruitment crisis. It will bring together a range of health and social care professionals to work together to provide enhanced personalised and preventative care for their local community. Focusing on local population needs, the aim is to provide care closer to patient's homes, before hospital admission may become necessary.
With an increased size and thus sustainability come different working patterns. This provides increased access but then impacts on perceived continuity. You cannot have one with the other. However, behind the scenes increasing systems are put in place whereby GP's are constantly communicating with each other about patient concerns, progress, improvement or deterioration and patient care plans and notes are routinely reviewed. There is still a single named GP for every patient who has overarching knowledge and understanding of their patients but they may lead a team that provides ongoing care, rather than run the team.
It is a fine line between offering unlimited on the day access and regular routine appointments and we must acknowledge that at times the balance can go either way, but it is with an understanding and open mind that we move things forward, learning from what we have achieved in the past to improve and redesign for the better in the future. We are in a time of significant change and all of the staff at Granta are looking to provide outstanding care for their patients. However, we can only do this with the support of our patients. We must adapt to patient's needs, always be open to suggestions, but maintain our desire to move the practice forward to what we believe it can become.
On Behalf of Granta Medical Practices
Dr Tim Wright
Chief Operations Officer


If you would like to add a club, society, news story, event or anything else to the website, please contact Clare Edwards on thebarleywebsite@gmail.com.